In a rare medical case, a 54-year-old male developed acute pancreatitis secondary to marijuana use. This case, documented in a recent report, highlights the potential adverse effects of cannabis on the pancreas. The patient, who used marijuana daily to manage chronic abdominal pain, presented with severe abdominal pain, nausea, and vomiting. Despite extensive testing, no other cause for his pancreatitis was identified, leading to the conclusion that his condition was induced by cannabis use.
Understanding Cannabis-Induced Pancreatitis
Cannabis-induced pancreatitis is an uncommon but increasingly recognized condition. The pancreas, an organ crucial for digestion and insulin production, can become inflamed due to various factors, including alcohol, gallstones, and, as emerging evidence suggests, cannabis. The active compounds in cannabis, THC and CBD, interact with cannabinoid receptors in the pancreas, potentially triggering inflammation. This interaction can lead to acute pancreatitis, characterized by severe abdominal pain, nausea, and elevated pancreatic enzymes.
The case report underscores the importance of considering cannabis use in patients presenting with unexplained acute pancreatitis. While alcohol and gallstones are the most common causes, cannabis should not be overlooked, especially as its use becomes more widespread. The patient in this case had no history of alcohol use, gallstones, or other common risk factors, making cannabis the likely culprit. This highlights the need for healthcare providers to take a thorough history of substance use in patients with acute pancreatitis.

Moreover, the report suggests that cessation of cannabis use can prevent further episodes of pancreatitis. The patient’s condition improved with supportive care, but his pancreatic inflammation persisted due to continued cannabis use. This case emphasizes the importance of patient education and the potential benefits of discontinuing cannabis in those with recurrent pancreatitis. As cannabis legalization expands, awareness of its potential adverse effects is crucial for both patients and healthcare providers.
Clinical Presentation and Diagnosis
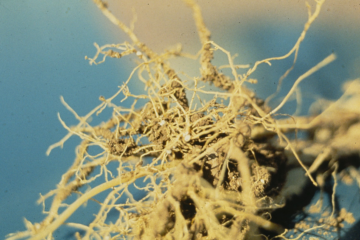
The clinical presentation of cannabis-induced pancreatitis can be similar to other forms of acute pancreatitis. Patients typically present with severe abdominal pain, often radiating to the back, along with nausea and vomiting. Laboratory tests usually reveal elevated levels of pancreatic enzymes, such as amylase and lipase. Imaging studies, including CT scans, can show inflammation and other changes in the pancreas. In this case, the patient had elevated lipase levels and CT findings consistent with severe pancreatitis, including pseudocyst formation and necrosis.
Diagnosing cannabis-induced pancreatitis requires a high index of suspicion, especially in patients with no other identifiable risk factors. A thorough history of substance use is essential, as patients may not readily disclose their cannabis use. In this case, the patient admitted to daily marijuana use, which was initially overlooked as a potential cause. This highlights the need for healthcare providers to ask specific questions about cannabis use and consider it in the differential diagnosis of acute pancreatitis.
The case report also emphasizes the importance of ruling out other causes of pancreatitis. The patient underwent extensive testing, including liver function tests, triglyceride levels, and imaging studies, to exclude other potential causes. This comprehensive approach is crucial for accurately diagnosing cannabis-induced pancreatitis and guiding appropriate management. In this case, the absence of other risk factors and the patient’s history of cannabis use led to the conclusion that his pancreatitis was cannabis-induced.
Management and Prognosis
The management of cannabis-induced pancreatitis is similar to other forms of acute pancreatitis. Initial treatment focuses on supportive care, including pain management, hydration, and nutritional support. In severe cases, hospitalization may be required for close monitoring and treatment of complications. The patient in this case received supportive care, including intravenous fluids and pain management, which led to gradual improvement in his symptoms.
Cessation of cannabis use is a critical component of management to prevent recurrent episodes of pancreatitis. The case report highlights that continued cannabis use can lead to persistent inflammation and slow recovery. Educating patients about the potential risks of cannabis use and encouraging cessation can significantly improve outcomes. In this case, the patient’s condition improved with supportive care, but his recovery was prolonged due to ongoing cannabis use.
The prognosis for cannabis-induced pancreatitis is generally favorable with appropriate management and cessation of cannabis use. Most patients recover fully with supportive care, although severe cases may have a more complicated course. The case report underscores the importance of recognizing cannabis as a potential cause of acute pancreatitis and providing appropriate education and support to patients. As cannabis use becomes more prevalent, awareness of its potential adverse effects is essential for improving patient outcomes.